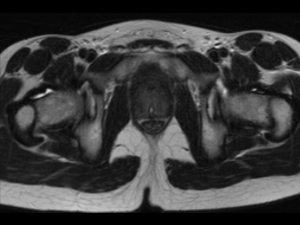
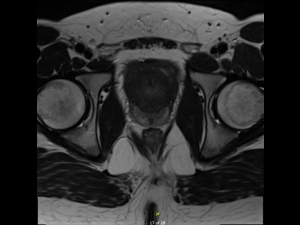
A 15-year-old male had been under the care of the paediatric urology team for long-term bladder outflow obstruction secondary to prostate enlargement for several years. He had had a previous transrectal ultrasound (TRUS) biopsy some years prior which had demonstrated no features of malignancy, but serial MRI scans had revealed progressive enlargement of the gland, such that there was sufficient concern to warrant a repeat biopsy. (See MRI images below)
This coincided with the development of the transperineal biopsy service at the patient’s local university hospital, with the obvious benefits of a more extensive, systematic biopsy and the reduced risk of associated post-biopsy infection. The patient was therefore planned for a systematic transperineal prostate biopsy under general anesthesia, utilising the FujiFilm Arietta 65 ultrasound system with biplanar transperineal ultrasound probe C41L47RP.



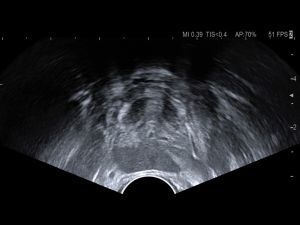
A four-quadrant systematic prostate biopsy was performed, obtaining four 20mm 18-gauge biopsies from each quadrant, totalling 16 cores in total. The histopathology demonstrated features of chronic inflammation on a background of features consistent with a rhabdomyoma. There were no features to suggest malignancy and as such the patient will be kept under surveillance, with no surgical management needed at this juncture.